Professor Gordon Guyatt, MD, MSc, FRCP, OC is a Distinguished University Professor in the Department of Health Research Methods, Evidence and Impact and Medicine at McMaster University. He is a Fellow of the Canadian Academy of Health Sciences.
The British Medical Journal or BMJ had a list of 117 nominees in 2010 for the Lifetime Achievement Award. Guyatt was short-listed and came in second-place in the end. He earned the title of an Officer of the Order of Canada based on contributions from evidence-based medicine and its teaching.
He was elected a Fellow of the Royal Society of Canada in 2012 and a Member of the Canadian Medical Hall of Fame in 2015. He lectured on public vs. private healthcare funding in March of 2017, which seemed a valuable conversation to publish in order to have this in the internet’s digital repository with one of Canada’s foremost academics.
For those with an interest in standardized metrics or academic rankings, he is the 14th most cited academic in the world in terms of H-Index at 240 and has a total citation count of more than 247,000. That is, he probably has among the highest H-Indexes, of any Canadian academic living or dead.
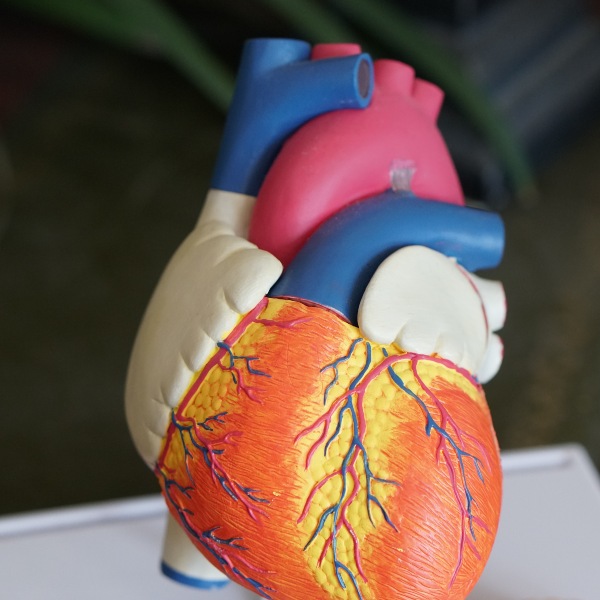
Scott Douglas Jacobsen: So, you have some areas of more applied research as opposed to guideline research. One of them deals with non-cardiac surgery leading to heart problems or creating extra problems. What is going on there?
Distinguished Professor Gordon Guyatt: So, first, to acknowledge that one of the guys who trained with me, he has now become an international research superstar. I am privileged to be working with him. His name is P.J. Devereux. He works at our institution here at McMaster University. He has become by far the leading worldwide investigator.
Jacobsen: What about the work that he’s done? Where is it going?
Guyatt: So, the first thing was that he recognized. There was a problem that we had not paid of attention to, and that problem is people undergoing surgery – not for their heart. So, they get a hip replacement. They get a colonoscopy. They may have a gall bladder problem. They have surgery for an ulcer. They have surgery for cancer.
All these non-cardiac surgeries. More and more, we do these surgeries in older people. So, in the past, if you were 90 years old, no way anybody would think of doing a hip replacement. Nowadays, 90-year-olds get hip replacements, appropriately, if they are active.
So, the population in whom we do surgery is older than it used to be, we do more extensive surgery. So, Albert Einstein died of a ruptured aortic aneurysm. Everybody knew he had an aneurysm. Nobody could do anything about it. Today, we have major surgery for people with ruptured aneurysms. We replaced their aorta the biggest blood vessel in the body. They do okay.
Jacobsen: Wow!
Gordon Guyatt: So, whereas, we are taking older people and with bigger surgery. The result of all that is some people have described it as a major surgery. That the stress it puts your body through is like running a marathon.
If you are 70-years-old and sedentary, that is probably not going to be such a great thing to suddenly be running a marathon. So, what happens is people have cardiac complications, heart attacks, they die of their heart attacks.
So, this non-cardiac surgery is the cardiac complications of non-cardiac surgery are a huge worldwide problem. It was a neglected problem, not too many people paid much attention to it. Dr. Devereux came along. He has a suspicion. The first thing he noticed as he checked it out. He was suspecting is that we were only seeing the tip of the iceberg.
The reason we were only seeing the tip of the iceberg was you go in and have surgery afterward and after surgery you come out; you your body has been assaulted in this major way. Inevitably, you have pain. You are given major pain-killers, narcotics.
They put you to sleep for a couple of days. You get through it. However, if you have had a heart attack during those couple of days, you may not have noticed it because you were under the narcotic. Then Aspirin was never the last. You suffer from the consequences of that heart attack, maybe even die from a cardiac arrhythmia of the heart.
The heart is not beating regularly or you end up with heart failure with your heart not pumping properly. You are short of breath. Your activities go down, and so on.
So, nowadays, we have what we call cardiac enzymes. So, when you have a heart attack, when your heart tissue dies because a blood vessel has closed off, the heart releases these enzymes. We can measure them sensitively nowadays.
What Dr. Devereux found out, we were missing 80 percent of the heart attacks. 80 percent of the heart attacks because the people were too sedated to tell us they were having one. So, normally, you are walking around. I have got chest pain. Right, so, you go to emergency. We do a cardiogram.
We check your enzymes. We say, “Yes, you are having a heart attack.” We might do emergency putting in of a stent in one of your blood vessels and giving drugs, and so on and so forth.
What happens when you have these narcotics after surgery, you are not awake enough to say, “Oh, I am having chest pain.” Nobody notices, nobody does the enzymes. Nobody notices that you’ve had a heart attack.
So, the first thing that Dr. Devereux did is he started looking to measure the enzymes after people had non-cardiac surgery. He found that we are missing 80 percent of the heart attacks. So, that was a big deal.
So, now, the world is changing its practice as we speak in response to Dr. Devereux’s work. Now, people are starting to look, but we do not know what to do with those heart attacks. They are different from the heart attacks coming through the emergency room.
So, 70s with a heart attack. What do we do? We could treat them the way we do. The people coming to emerge, but we were not so sure about it anyway. Devereux ‘s latest study has shown that giving these people anticoagulants thinning blood thinners, as we call them, after their non-cardiac surgery reduces their major cardiac events.
It strongly suggests that we should be giving aspirin, for instance; that we give it to people with heart attacks in the emergency room after you’ve had these heart attacks after cardiac surgery. He is in the start of his program.
We will be thinking of how to prevent these heart attacks. He’s already done one of his first studies showing that a drug that everybody thought would prevent heart attacks, prevented the heart attacks, but caused strokes.
It, in fact, probably increased deaths, which is not such a good idea. So, he’s leading the world in this work. Eventually, it is changing worldwide practice. In the end, people are going to do much better in terms of not having heart attacks or having them treated properly, when they have non-cardiac surgery.
Jacobsen: Thank you for the opportunity and your time, Professor Guyatt.
We conducted an extensive interview for In-Sight: Independent Interview-Based Journal before: here, here, here, here, here, and here. We have other interviews in Canadian Atheist (here and here), Canadian Science (here), Canadian Students for Sensible Drug Policy, Conatus News, Humanist Voices, and The Good Men Project (here, here, here, here, here, here, here, here, here, here, and here).
Photo by Robina Weermeijer on Unsplash